Insight
The Complete Guide to Conversational AI Agents for Patient Access

A practical playbook for leaders rolling out AI agents across phone, chat, and text
Patient access is the front door to care. And right now that front door is… jammed.
Call volumes are up. Staffing is tight. Hold times are brutal. Agents are burned out. Patients are frustrated. And every dropped call is a missed appointment, a delayed diagnosis, or a patient who goes elsewhere.
That’s why patient access leaders are turning to conversational AI — not as a shiny tech experiment, but as an operational strategy.
This guide is for patient access leaders who want to answer one question:
“How do we roll out an AI patient access agent safely, effectively, and with measurable ROI?”
Let’s break it down.
What is Conversational AI for Patient Access?
Conversational AI is software that can interact with patients using natural language through:
- Phone (voice)
- Web chat
- SMS/text
- Patient portals
- Mobile apps
But here’s the key:
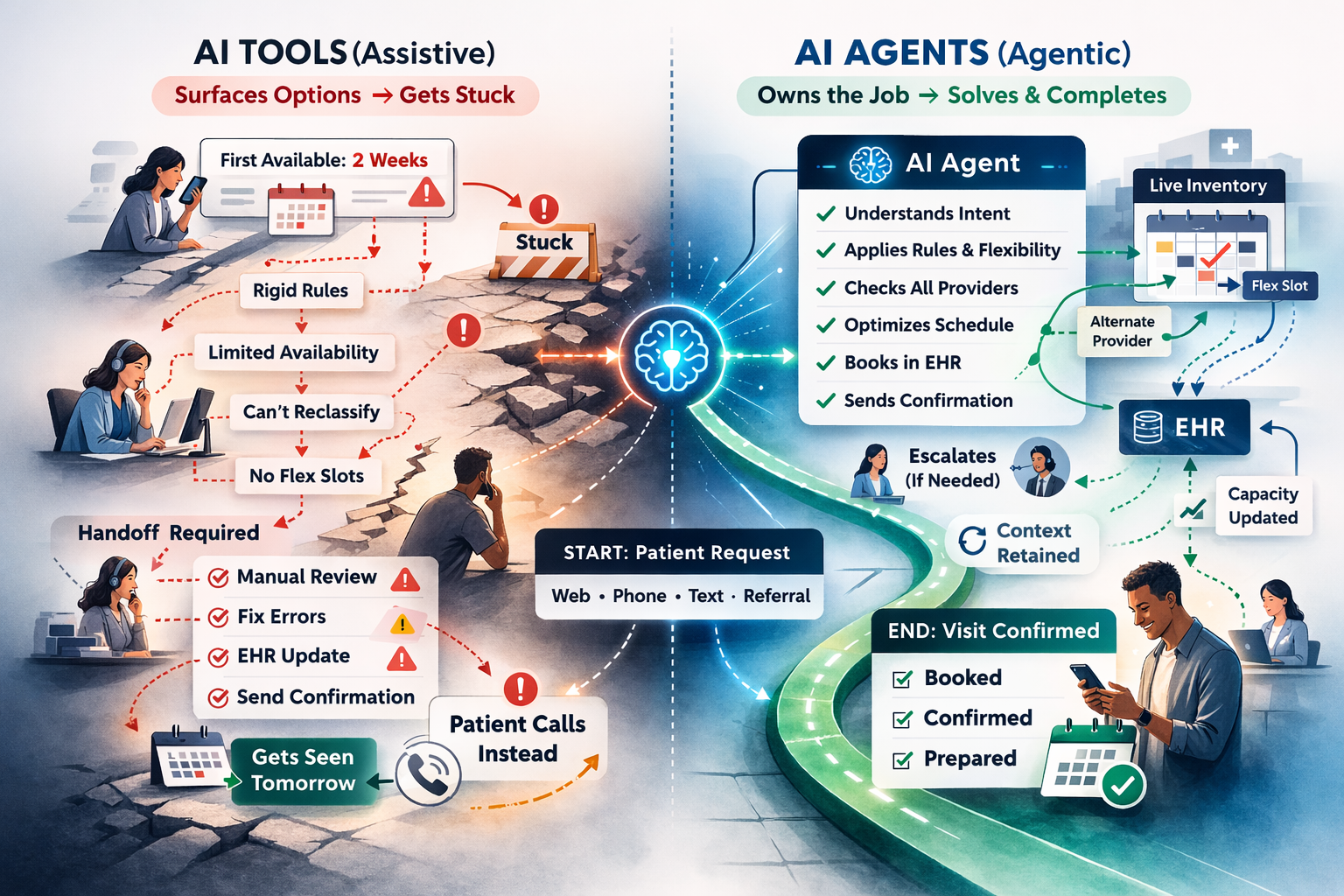
Modern conversational AI isn’t just “chat.” It’s task completion.
A real AI patient access agent doesn’t just say helpful things. It can:
- Schedule appointments
- Route calls
- Collect patient info
- Answer common questions
- Confirm, cancel, or reschedule
- Send instructions and reminders
- Escalate to a human when needed
The goal isn’t “automation for automation’s sake.” The goal is faster access, better patient experience, and less pressure on staff.
Why Patient Access Leaders Are Implementing AI Agents Now
1) Call volume isn’t going down
Patients still prefer calling for high-stakes needs:
- “I need an appointment today”
- “I’m confused about my bill”
- “I don’t know what to do next”
- “I need to talk to someone”
2) Staffing shortages are real (and persistent)
Even the best-run access centers are fighting:
- turnover
- training time
- seasonal spikes
- coverage gaps
3) Access performance is now a strategic KPI
Patient access is no longer “front desk operations.” It’s tied directly to:
- leakage
- growth
- experience scores
- clinical outcomes
AI is one of the only levers that scales without hiring.
What a Great AI Patient Access Agent Can Do (Use Cases That Actually Matter)
The highest value use cases aren’t the flashiest ones. They’re the ones that reduce call burden and improve throughput.
1) Appointment scheduling + rescheduling (the big one)
AI can support:
- new patient scheduling
- returning patient scheduling
- rescheduling/cancellations
- provider/location selection
- appointment reminders
Why it matters: Scheduling is high volume, repetitive, and measurable.
2) Call routing that actually works
Instead of “Press 1 for… Press 2 for…”
AI can ask:
“What can I help you with today?”
Then route based on:
- intent (scheduling, billing, results, referrals)
- urgency
- patient type
- clinic rules
Why it matters: Routing failures create transfers, hold time, and abandonment.
3) FAQs + operational questions (low risk, high deflection)
Examples:
- clinic hours
- directions / parking
- prep instructions
- insurance accepted
- how to get records
- portal help
Why it matters: This stuff eats up human time and doesn’t require humans.
4) Intake + data capture before the visit
AI can collect:
- demographics
- symptoms (non-emergent)
- reason for visit
- preferred location/provider
- insurance details (where appropriate)
Why it matters: Better intake = faster scheduling + cleaner handoffs.
5) Referral coordination support
AI can:
- explain referral requirements
- collect info
- route to the right team
- update status (if integrated)
Why it matters: Referrals are a common drop-off point for patients.
The Business Case: What ROI Looks Like (And What to Measure)
If you’re going to roll this out, don’t measure “AI conversations.” Measure operational outcomes.
Core KPIs patient access leaders should track
Access & Experience
- Call abandonment rate
- Average speed to answer
- Average hold time
- Patient satisfaction / NPS / CSAT
Efficiency
- Containment rate (resolved without human)
- Transfers per call
- Average handle time (AHT)
- After-call work time
Growth & Revenue
- Appointments booked
- Appointment conversion rate
- No-show rate (pre vs post)
- Leakage reduction (where measurable)
Quality & Safety
- Escalation rate
- Error rate / correction rate
- “Human rescue” rate
The simplest ROI formula
ROI = (Labor hours saved + additional appointments captured) – total program cost
Leaders don’t need perfect math. They need directional truth and a plan to prove it.
What Makes an AI Agent “Enterprise-Ready” (Not Just a Bot)
Here’s the brutal truth:
A lot of tools demo well. Very few survive the chaos of real patient access.
Non-negotiable capabilities
1) Accurate intent detection
Patients don’t speak in workflows. They speak in chaos.
2) Human handoff that preserves context
If the AI transfers the call, the human should see:
- why the patient called
- what was collected
- what was attempted
3) Strong guardrails
The agent must know when to say:
- “I’m going to connect you with a team member.”
- “If this is urgent, call 911.”
4) Integration strategy
Best case: scheduling + patient data integration
Minimum case: routing + data capture + handoff summary
5) Reporting and analytics
If you can’t measure it, you can’t improve it.
Safety, Compliance, and Risk (The Stuff That Makes Leaders Nervous)
Good. You should be nervous. This is healthcare. You don’t get to be reckless.
The biggest risks to plan for
Hallucinations / incorrect answers
AI must not “guess” clinical guidance or policy.
Inappropriate triage
The agent must have strict escalation rules.
PHI handling
You need clarity on:
- what data is collected
- where it’s stored
- how it’s protected
- how long it’s retained
Unclear ownership
If something goes wrong, who owns it? Patient access? IT? Compliance? Clinical ops?
Best practice: define a governance model upfront
At minimum, establish:
- an executive sponsor
- operational owner (patient access)
- IT/security owner
- compliance review
- clinical escalation input
The Rollout Playbook: How to Implement Without Breaking Your Operation
This is where most organizations mess it up:
They try to do everything in month one.
Don’t.
Phase 1: Pick one high-volume workflow (2–4 weeks)
Choose a use case with:
- high call volume
- repeatable steps
- low clinical risk
- clear success metrics
Great starters:
- appointment scheduling (specific clinics)
- rescheduling/cancellations
- clinic FAQs
Phase 2: Pilot + measure (4–6 weeks)
Define success before you launch.
Pilot goals should include:
- containment rate target
- reduction in abandonment
- patient experience baseline
- staff feedback loop
Run weekly reviews:
- what failed?
- what escalated?
- where did patients get stuck?
Phase 3: Expand scope (6–12 weeks)
Once you’ve proven value, expand to:
- more specialties
- more locations
- more channels (voice + SMS + chat)
- more complex workflows (referrals, intake)
Phase 4: Optimize like a product (ongoing)
AI is not “set it and forget it.”
Treat it like a living program:
- new intents appear
- policies change
- scheduling templates shift
- patient behavior evolves
The organizations that win build a continuous improvement loop.
Vendor Evaluation: Questions Patient Access Leaders Should Ask
Here’s your cheat sheet for demos and RFPs.
Workflow & performance
- Can the agent complete scheduling end-to-end?
- What’s the real containment rate in production environments?
- How does it handle ambiguity and multi-intent calls?
Escalation & handoff
- What triggers escalation?
- Does the agent transfer with full context?
- Can it route to the right queue/location/team?
Integration
- What EHR/PM integrations exist today?
- What’s required from our IT team?
- What’s the fallback plan without integration?
Compliance & security
- How is PHI handled and protected?
- What’s logged? What’s stored? What’s deleted?
- What controls exist to prevent unsafe responses?
Reporting & ops
- What dashboards do leaders get?
- Can we track containment, abandonment, scheduling conversion?
- How do we review failures and retrain?
Change Management: The Part Nobody Plans For (But Always Matters)
You’re not just rolling out software. You’re changing how access works.
How to get staff buy-in
Tell the truth:
“This isn’t replacing you. It’s taking the repetitive stuff so you can focus on patients who need a human.”
Involve frontline staff early:
- listen to objections
- build escalation rules together
- let them shape workflows
How to position it to patients
Don’t pretend it’s human. Patients hate that.
Try:
“I’m an automated assistant here to help you schedule, get answers, or connect you with the right team.”
Clarity builds trust.
Common Mistakes (So You Don’t Step on the Same Rakes)
Mistake #1: Trying to automate everything
Start narrow. Win. Expand.
Mistake #2: Measuring the wrong things
“Number of conversations” is meaningless. Measure outcomes.
Mistake #3: Weak escalation logic
The AI must know when to stop.
Mistake #4: Ignoring the contact center reality
Peak times, staffing rules, queues, and transfers matter more than fancy AI.
Mistake #5: Treating AI like a one-time implementation
It’s a program. It needs ownership.
What to Do Next (A Simple 30-Day Plan)
If you’re a patient access leader evaluating AI, here’s your move:
Week 1: Baseline your access metrics
- abandonment
- hold time
- top call drivers
- scheduling conversion
Week 2: Pick your pilot workflow
Choose one use case with clear success criteria.
Week 3: Define governance + escalation rules
Get alignment across:
- patient access
- IT/security
- compliance
- clinical stakeholders (if needed)
Week 4: Launch a controlled pilot
Measure weekly. Improve fast. Don’t overcomplicate it.
Bottom Line
AI patient access agents aren’t the future. They’re the present.
The organizations that win won’t be the ones with the flashiest tech. They’ll be the ones who roll it out like operators:
- pick the right workflow
- measure outcomes
- protect safety
- scale with discipline
If you do that, you don’t just reduce call volume.
You unlock access.
More Articles
Insight
AI Agents in Patient Access: What’s Real, What’s Hype, and Why It Matters
Insight
The Complete Guide to Conversational AI Agents for Patient Access

Insight
Designing responsible guardrails for Healthcare AI agents